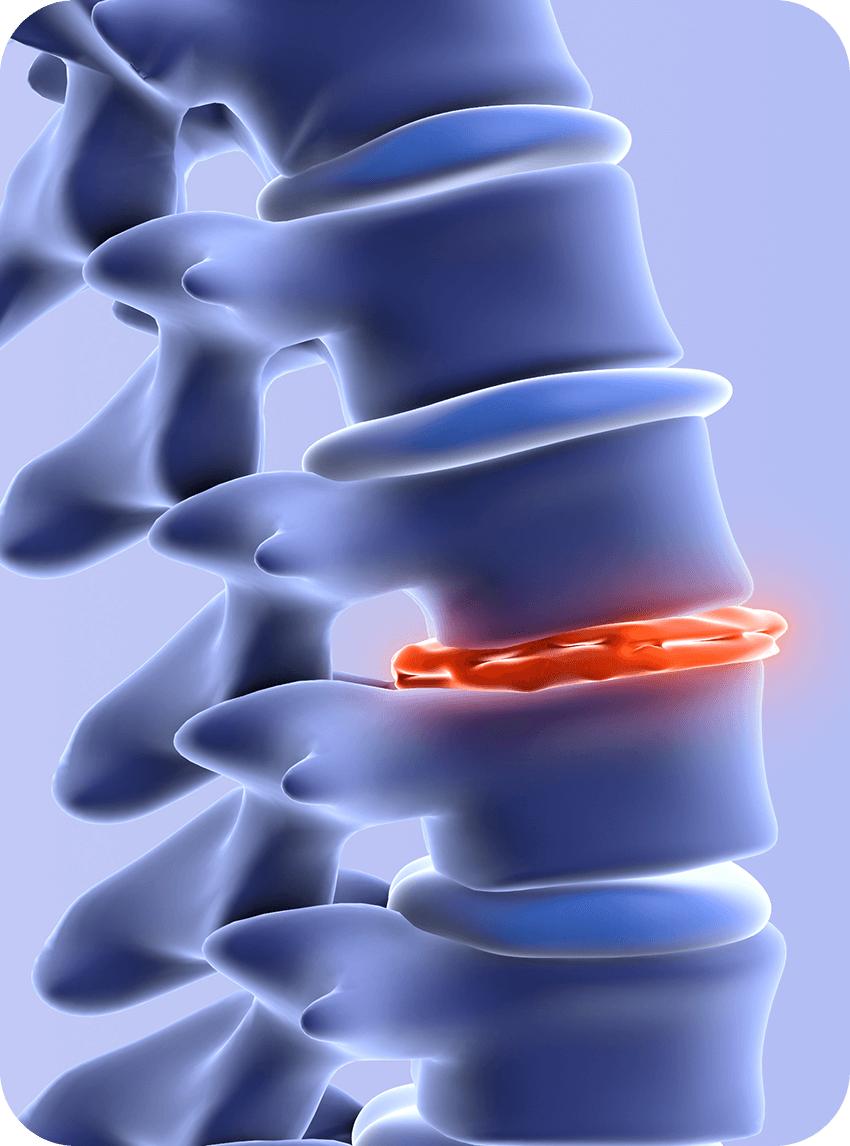
Degenerative Disc Disease
Your spine is made up of bones (vertebrae) separated by discs that act as cushions. These discs provide flexibility, absorb shock, and protect the spinal column. Over time, discs can dry out, lose height, or become damaged. When this happens, they don’t function as effectively, which can irritate nearby nerves or place extra strain on surrounding joints. This process is referred to as Degenerative Disc Disease.
Degenerative Disc Disease develops gradually and may be influenced by several factors:
- Aging – natural changes that cause discs to lose hydration and elasticity
-
Injury or trauma – damage to the spine can accelerate degeneration
-
Genetics – some people are more prone to disc problems
-
Repetitive strain – heavy lifting, twisting, or certain sports can put extra stress on discs
-
Lifestyle factors – smoking, obesity, and poor posture can speed up degeneration
Symptoms vary depending on which part of the spine is affected, but may include:
-
Chronic or recurring back or neck pain
-
Pain that worsens with sitting, bending, or lifting and improves with walking or lying down
-
Stiffness and decreased flexibility in the spine
-
Radiating pain, numbness, tingling, or weakness in the arms or legs if nerves are compressed
Injections of corticosteroid medication around the irritated nerves can decrease inflammation and provide temporary relief, making physical therapy more effective. Learn more about Epidural Steroid Injections.
When arthritic joints around the disc are the main pain source, RFA can interrupt pain signals from specific nerves, offering longer-lasting relief. Learn more about Radiofrequency Ablation (RFA).
Reserved for severe cases, surgery such as spinal fusion or artificial disc replacement may restore stability and reduce pain.